Hear Mark read this post — subscribe to Lean Blog Audio
Just over a year ago, I had an opportunity to spend a day with some Lean leaders at the famed Cleveland Clinic. My hosts included Nate Hurle and Dr. Lisa Yerian. They have both been sharing a lot of great material on Twitter this year, so check out their profiles and follow them.
I had a chance to visit one of their community hospitals, Hillcrest Hospital, as well as the main campus. It was a very stimulating visit and it was great to see the progress they were making in building a “culture of improvement.”
Nate and Lisa encouraged me to write about what I saw… and I meant to… and they followed up (in a friendly way)… there's really no good reason why it took me a year to write more about the visit. Maybe I had too much WIP in my head, as my friend Jim Benson would say. Better late than never…
Here are two posts that I did write, from January, about the Cleveland Clinic Improvement Model:
So what else did I see that day? I saw many really encouraging signs of culture change. I saw engaged leaders at all levels and staff members who were excited about driving improvement.
One positive was, quite literally, a sign that expresses an important notion for Cleveland Clinic to build upon… a big sign that talked about putting patients first.

Putting patients first is, of course, very compatible with the Lean philosophy of putting customers first. So, an organization that already has a very high level of focus on patients' needs and the patient experience seems likely to do better in embracing the Lean approach than an organization that still orients everybody around the doctors.
Signs like this, of course, have to be more than just a slogan. It needs to be something that an organization lives up to each and every day.
Getting Input From Staff About Goals
At the Cleveland Clinic sites, I visited many departments that had standardized boards for daily management, including performance metrics and improvement activity. That's all becoming more common in healthcare these days.
One thing that stood out as being unusual (in a good way) was hearing leaders in different departments talk about staff members giving input into their goals. In a way, this sounds like the Lean concept of “catchball” where goals are no longer just dictated in a top-down way. Staff giving input leads to discussion and consensus building in a Lean culture.
In my own past consulting projects, when I've asked hospital staff an open ended question like, “What should we improve?” or “What goals are we trying to achieve?,” the answers from front-line staff generally haven't been that far off from what the managers would say. I remember a microbiology department team that talked about turnaround times for lab results and the need to reduce overtime (they were tired and overworked). That lined up with exactly what management was looking to accomplish (although they were driven a bit more by cost reduction).
Asking staff for input (and taking that input seriously') helps people feel respected — because they ARE being respected.
Different Modes of Improvement
In the Cleveland Clinic departments, they were taught different modes of improvement. Not everything needs to be an A3 and not everything needs to be a formal Rapid Improvement Event. When staff are engaged to point out problems and focus on improvement, Cleveland Clinic teaches them various approaches that can be used on problems of different size and complexity.
Dr. Yerian says:
We tend to roll these [methods] out all at once. We find that when we introduce waste and ask them to identify waste in the work or “what gets in the way,” they identify a spectrum of wastes and problems that require all three approaches. And then we're off…”
They use relatively simple Kaizen Cards and more complex A3 problem solving templates. But, it's all Plan-Do-Study-Adjust (PDSA), as Joe Swartz and I wrote about in Healthcare Kaizen.
They utilize root cause analysis techniques, including fishbone diagrams (I saw many of those posted) and “the 5 whys,” as needed. Some improvements are “Just Do Its” or “Quick and Easy Kaizens.” I'm all for not overcomplicating things and Cleveland Clinic seems to agree.
The teams focus on a single A3 at a time, receiving assistance from a coach, which seems to be a really important success factor.
The goal, as stated by Cleveland Clinic, is to have a “culture of improvement.” Working toward that culture takes time. It's a journey. You don't “implement” a new culture overnight. It takes coaching and leadership over time… but they seem to be working on it.
Environmental Services
One of our first stops in our Gemba visits was to meet staff in the EVS department to hear about their improvement work.
Members of their team gave a series of short stand up presentations about problems they had solved in their work. They were focused on simplifying and improving what they did and how they did it.
One staff member presented about their process for providing key and badge access to employees and managers. They learned, when they dug into the details of the work (something that most people don't get the chance to do), that there were 65 different access point profiles, which they decided was overkill. They weren't short cutting security through this effort, they made this clear. They got it down to 13 different profiles, and then just three. They found “a simpler way.”
I was also impressed that the team was learning to “look at the process, not pointing fingers at people.”
They talked about other improvements. The details of the improvements mattered to them, but I was more taken aback with how well they seemed to understand and articulate Lean culture concepts. They were talking about “countermeasures” (instead of “solutions”), using the 5 whys (or whatever the right number of whys is), and more.
They talked about developing “80% solutions” instead of talking forever in the name of a perfect solution. As they said, “We might not have solved it, but lessened the effect and we keep working at it. We don't jump to solutions.”
When somebody mentioned that the EVS department had only been on their Lean / improvement journey for six months, I was really surprised. “Just six months?” I was really impressed.
The EVS department and their efforts show that Kaizen really is for everybody. The ability to study and improve one's work doesn't have much to do with your formal education. Everybody can be an expert in how their own work is done. Everybody has the potential to be creative and to improve their work, especially when they are taught and coached on these concepts.
Patient Transport
In this department, I remember how enthusiastic the team lead was about improvement. He and the other two team leads were designated as coaches for improvement activity in the area.
The team lead said they asked, early on, “We're already high performing… so why process improvement?” They came to realize that there's always room for improvement and that it can be energizing.
Their team was also asked for input on finding waste and what was important to the team and their customers.
They talked about “going from band-aids to root cause.” Their powerful summary statement was:
“Our voice is heard and we can make a difference. We study the work, we see what's possible.”
This all goes to show that Lean, of course, is not about managers or experts telling people how to do their work differently. It's a process for engaging those who do the work, providing coaching and being partners in improvement. That was so great to see.
Nursing Units
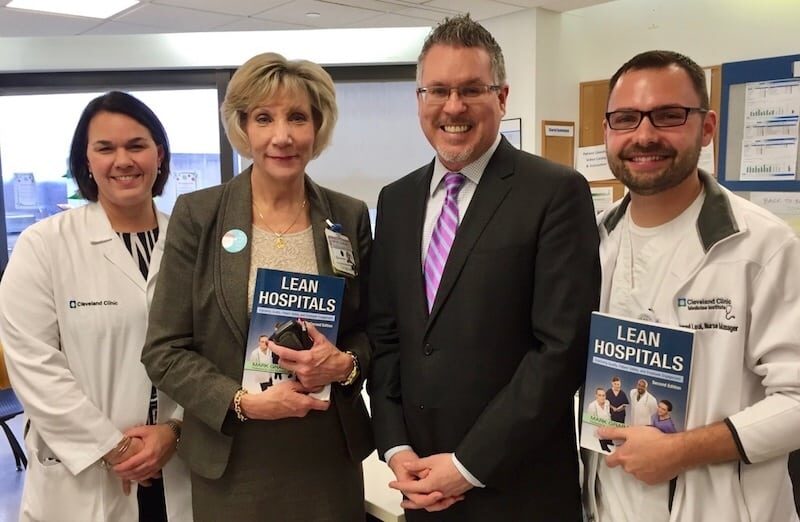
Here's a picture of some nurses and staff who wanted a picture with me and their copies of Lean Hospitals (the 3rd edition was not out yet):
In the NICU, staff talked about their change process, which included formal “stakeholder analysis” (something that's often neglected… and something participants get to practice in my change management workshop).
Another unit (“5 main,” a med/surg floor) had saved $177,000 through Kaizen improvements and were also improving patient care. Patient satisfaction surveys about “staff responsiveness” showed huge improvements from what was sometimes the first percentile (very low) to the 99th percentile (very high performance).
Phlebotomy
There were many other places that we visited. I went through day not expecting to blog about my visit, so my notes trailed off apparently. I remember the phlebotomy (specimen collection) area being very proud of their improvements.
Here is a video about some of that work that I saw (with CEO Dr. Toby Cosgrove going to see):
Before, they were only seeing about 50% of their patients within 15 minutes (their goal was to see 95% within that time). They're now often at 100% performance.
These results didn't come from pressuring staff to work faster; they made a number of systemic improvements to the way work was structured and performed.
Everybody Finding a Better Way
In these various departments, staff and leaders were holding huddles and having discussions about improvement. In their “daily accountability” discussions, they're all asking “what's preventing us from _____?” instead of pointing fingers and blaming people for poor performance. Those mindsets and behaviors help build this culture of improvement.
One employee said:
“Before, the executives had the answers. Now, we involve everybody.”
That's always great to see. The excitement and positive attitudes were very noticeable. My visit to Cleveland Clinic was energizing and reinvigorating.
I hope that Nate and Lisa will write a guest post talking about the progress they made in 2016.
What progress is your organization going to make toward becoming (or strengthening) a culture of improvement in 2017?
What do you think? Please scroll down (or click) to post a comment. Or please share the post with your thoughts on LinkedIn – and follow me or connect with me there.
Did you like this post? Make sure you don't miss a post or podcast — Subscribe to get notified about posts via email daily or weekly.
Check out my latest book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation:




![Marcia Daszko on Leadership Lessons from Dr. Deming; Pivot Disrupt Transform [Podcast]](https://www.leanblog.org/wp-content/uploads/2024/03/lean-blog-501-marcia-daszko-238x178.webp)



Thanks Mark – it’s great to get a glimpse of what you see in our gemba! We’d be happy to contribute to your blog! What type of share would provide the most value to your readers?
Thanks, Lisa for your openness and transparency. I’m curious what questions the readers might have.
Some related tweets, one related to today’s podcast episode #270 on burnout: