This article in The Wall Street Journal caught my eye the other day:
Can Tech Speed Up Emergency Room Care?
At first I thought, “Oh, this is a rural E.D. where they need to use telemedicine to bring specialists to the patient virtually?”
No, it's NewYork-Presbyterian/Weill Cornell Medicine in Manhattan.

Wait, they don't have emergency physicians?
They do, but they're down the hall.
From the article, which emphasizes technology in the headline:
“Dr. Greenwald was talking through a computer screen. Mr. Winter–a 75-year-old construction-company consultant who had suffered a number of injuries from a fall the previous week–was sitting in a small, private room in the hospital's emergency department, elsewhere in the complex.”
OK, so “elsewhere in the complex” not “down the hall.” Big hospitals have long hallways, so maybe it is a ways down the hall.
What's the goal?
“The goal: to reduce waiting times and get patients with non-urgent cases in and out of the emergency room efficiently without compromising care.”
That's a great goal. Better flow and better efficiency with the same quality (if not better quality as a direct result of the shorter waiting times).
Non-urgent cases…
Fast Track / Split Flow Process Change
Ah, so the hospital has added what's either called a “fast track” or “split flow” E.D. This has become more common in recent years and is often considered a “Lean” practice (or it's adopted by hospitals that are “Practicing Lean“).
Read about an example of “Split-Flow” care here.
“The Split-Flow model of care is an evidence-based best practice that hospitals nationwide are adapting with the goal of shortening the time before a patient is seen by a physician or care provider, as well as the overall length of time spent in an emergency department. Long emergency department wait times are a major reason for low patient satisfaction scores and increase the potential of a patient leaving before receiving medical care. Split-Flow represents the commitment at St. Mary to provide the highest standards in quality care.
Using the Split-Flow Model of care, patients are first seen by a nurse immediately upon entering the Emergency Department. The nurse will make an initial evaluation and directs patients to Pediatric, Prompt Care, Acute Care, or an Expedited Treatment Area (ETA). Prompt care is for minor injuries or conditions, such as a sprained ankle or flu; and acute care is for those with severe illness or conditions who are likely to be admitted to the hospital. Pediatrics, Prompt and Acute care are most familiar to people using emergency services and it is the commitment to getting them seen by a physician within a remarkably reduced time frame that is part of the new restructuring process in the St. Mary emergency department.”
The lower-acuity patients are sent to what's basically an “urgent care” area. There are two (or more) separate value streams and patient flows. The high-acuity (most urgent) patients don't prevent the lower-acuity patients from also getting care.
Dr. Joe Guarisco (who I interviewed in Podcast #160) has been involved with Fast Track implementations, as you can read about here.
Cleveland Clinic has implemented “Split Flow” as you can read about here.
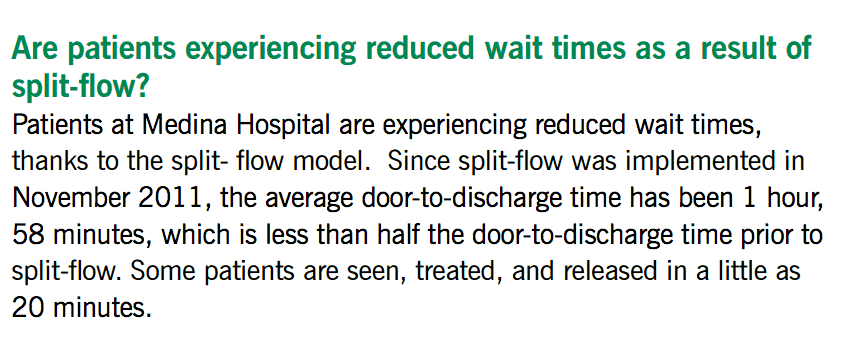
They've seen some dramatic reductions in waiting times:
My Healthcare Kaizen co-author, Joe Swartz, helped implement a system like this at his health system, among other improvements that were made. They did a “Fast Track” system for low acuity patients in 2007, then added “Split Flow” that adds mid-acuity patients to the mix.
Joe told me:
“About 60% of our patients now go through the less acute / ambulatory path.”
I've never heard of the use of telemedicine in any of these Fast Track / Split Flow success stories (in the U.S. or Canada). They were examples of system redesign and process improvement.
Of course, we can (and should) ask the important big-picture questions about why non-urgent patients are coming to the “emergency room.” It's not just about insurance. I've seen long waiting times in Canada, England, and Sweden, for example… the problem there was it being too difficult to get a primary care appointment promptly or at a convenient time.
The WSJ has written about Fast Track before:
Hospitals Cut ER Wait Time With New ‘Fast-Track' Units
“A growing number of hospitals are putting patients with relatively minor ailments — those who previously would be left to languish in the waiting room — into “fast track” units to get them in and out of emergency beds quickly.”
I don't think telemedicine was a part of that story. It was process change. They got good results. Good for them.
So What About Technology?
Back to Manhattan and the WSJ story… they've gotten good results. So, again, good for them. But it's a different approach (which is OK, but let's examine it):
“For patients who have opted to use the Express Care program–only offered to patients with minor injuries or complaints–the total amount of time spent in the ER has dropped to 35 to 40 minutes, from an average of 2 to 2.5 hours, he says.”
Two data points aren't a trend, but that seems like a statistically-significant difference. It's better.
But why? Because of the split flow or because of telemedicine? If they implemented both at the same time, it's hard to tell.
Their improvements and reductions in waiting times are about the same as what they saw at the Cleveland Clinic facility.
Is there an additive effect from telemedicine? The article says so, but we don't know how much:
“Meanwhile, doctors can now treat patients from more than one hospital from their desk, and pivot to their administrative tasks more quickly in between visits.”
We could (and should) ask why their administrative tasks take so long in between visits… but that's a different process improvement for a different blog post.
Hands-on care can't be done via video, of course…
“Though patients are connected to an ER physician through videoconferencing, often a nurse practitioner or physician assistant is on hand to assist or conduct procedures, such as removing stitches or ordering X-rays. The doctor will order prescriptions and print out discharge papers that are spit out from a printer in the patient's room.”
I'd share a similar concern… which doesn't mean this approach is worse… but I'd be concerned:
“Critics of telemedicine have raised questions about quality of care being sacrificed for convenience, as well as the impersonal nature of a virtual care.”
If I lived in the middle of nowhere, I'd appreciate telemedicine. I might not feel as plussed about it if the doctor was in the same zip code.
My concern is that technology is sexy. It seems like NewYork-Presbyterian/Weill Cornell Medicine implemented BOTH technology and process change.
Will others really understand that? Will they be tempted to think the technology is a silver bullet?
Will technology be more readily copied and adopted than process change?
Maybe that would be OK if the process change came along with the technology.
“Dr. Sharma has gotten inquiries from more than a dozen hospitals and health-care systems curious about the program.”
Ah, the benchmarking trip. Hospitals will often more readily invest in benchmarking trips instead of their own local process improvement and redesign efforts. A trip to NYC sounds amazing, though.
“Ali Raja, vice chairman of the department of emergency medicine at Massachusetts General Hospital, visited Weill Cornell's Express Care earlier in March.
“Ten years from now, tele-emergency medicine will be the standard around the country,” Dr. Raja says. “We'll still have emergency departments for those patients who are critically ill, but I think we're all headed in this direction.””
Doesn't that seem like quite a leap to think everybody will be doing this in 10 years?? Would that really be a good thing? Is it necessary?
Can we get those gains without telemedicine and it's possible downsides?
What do you think?
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s work together to build a culture of continuous improvement and psychological safety. If you're a leader looking to create lasting change—not just projects—I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s start a conversation.








![What’s Your Organization’s Real Mistake Policy? [Poll]](https://www.leanblog.org/wp-content/uploads/2025/07/Lean-Blog-Post-Cover-Image-2025-07-17T085114.134-100x75.jpg)

Mark, you have pointed out quite eloquently the seductive allure of a ‘solution’- something that fixes a problem- the question as always is: who’s problem.
But caring for all the patients in an ED is not a problem; it is a dilemma- a constant balancing act among valuable, but competing options with limited resources. The ‘benchmark’ ‘solution’ sounds great, but diverts attention away from the often difficult and messy balancing act, negotiation, and arbitration that must go in to choices about how to deploy those limited resources. And such a focus on a tech solution diverts limited capital away from developing a real strategy that actually improves the circumstances. That takes people working together, first identifying a shared outcome everyone is willing to work towards and then spending the time and energy to work out the logistics and discover the ‘better’ way to get the work done. This recognition and the energy to do this are often the missing links.
Although technology can certainly enhance process, technology cannot overcome unproductive process..at least not at a sustainable cost.
I agree that technology CAN enhance a good process. What I read, from the WSJ article and not going to the Gemba, is that the hospital didn’t get magic results from technology. It sounds like they improved the process AND used technology.
I’m just not sure the technology was necessary.
I wonder, also, if patients REALLY like seeing the doc on screen or if the hospital is cherry picking patient comments to rationalize their technology decision?