Today's Post in <50 Words: I get worked up about labeling a troubled surgical department as “a factory,” but there are far more important issues of patient safety and hospital culture to be discussed related to a Seattle Times investigative piece.
Next week is the annual Society for Health Systems Conference. See past blog posts from previous conferences.
I'm attending and participating again, as I do most every year. It's a great event that's focused on process improvement. Let me know if you're attending and please say hello. Follow on Twitter via the hashtag #SHS2017.
Since SHS is part of the Institute of Industrial and Systems Engineers, many of the attendees, like me, have worked in both manufacturing and healthcare.
We're able to see parallels and differences between the settings and understand how process improvement and leadership principles are transferrable across industries. We're working to make hospitals better hospitals. That doesn't mean “turning them into a factory” as people might fear in healthcare.
I understand when healthcare people have trouble seeing what would be transferrable, especially when many of them have never set foot in a factory. They don't know “what good looks like” in manufacturing. They wouldn't necessarily know the difference between a modern Lean factory that you would want to learn from and a bad, traditionally-run factory (like my GM plant was in 1995).
Hear Mark read this post (subscribe to the podcast series):
I get frustrated, though, when people make broad generalizations about factories being backward or crappy workplaces, as I blogged about here:
I read with interest when this Seattle Times article invoked the term “factory” when writing about a hospital and a surgeon (and a management team?) who are accused of putting quantity before quality.
My GM factory, sadly, did that in 1995. I've seen that outdated mindset in other factories that were still early in their Lean transformation.
But, we need to distinguish between “factory” as a general term and “bad factory.”
See this investigative piece from the Seattle Times that is interesting on many levels… it refers to the “O.R. Factory” as if all factories are sweatshops that crank out poor quality products. Again, that's as unfair as saying all bankers are crooks or that all restaurants would give you food poisoning.
In the article, the word “factory” doesn't get used. The word “Lean” thankfully doesn't enter the discussion. People sometimes incorrectly think Lean means pressuring people to work faster. No, Lean is actually the opposite of that old mindset and approach. Lean puts quality first and truly empowers people to do improve quality.
I suggest you read the article.
I shared some quotes from the article via Twitter, as I was reading it, including:
In a nutshell, the accusations (and counter claims are):
- A surgeon, Dr. Johnny Delashaw, is accused of prioritizing money, quantity, and volume over clinical best practice and quality (he denies that)
- Many staff members and other surgeons have quit or complained about his practice and behavior (the surgeon claims they are jealous or resistant to culture change)
- The surgeon payment model has been changed from pooling some revenue to encourage teamwork to a strictly individual RVU payment scheme
- It's alleged that a state law meant to encourage patient safety is being used (through a loophole) to force nurses to work 20 hours in a 24 hour period
- Some claim they are afraid to speak up in M&M reviews (but the surgeon claims he is not a bully)
- Poor outcomes are blamed on the surgeon having concurrent cases or being in clinic while “his” patients are in the O.R. being worked on by residents or other surgeons
- Delashaw was promoted into a leadership role, despite concerns that were raised by colleagues
- Hospital leadership seemed to diminish or ignore the allegations
There are a lot of concerns and problems here that you'd hope hospital leaders would take seriously.
Calling a bad hospital a “factory” doesn't shed any light or help the discussion. The problem is putting quantity over quality, as the article accuses them of. I'd criticize a factory or a hospital (or any organization) for doing that.
In a follow up to the investigation, we have this news:
“Swedish Health Services CEO Tony Armada has resigned, days after a Seattle Times investigation examined turmoil and troubles inside Swedish's premier neurosurgery institute.”
That article also has a shorter synopsis of the investigation.
“The Times reported that doctors have expressed concerns to Armada and other administrators about patient-safety issues at the neurosurgery institute, particularly when it came to Delashaw. Ten surgeons and staff members met with Armada in October, with some making desperate pleas to remove Delashaw, to detail their concerns about the shifting culture at Swedish, according to minutes from that meeting obtained by The Times.”
The meeting minutes include:
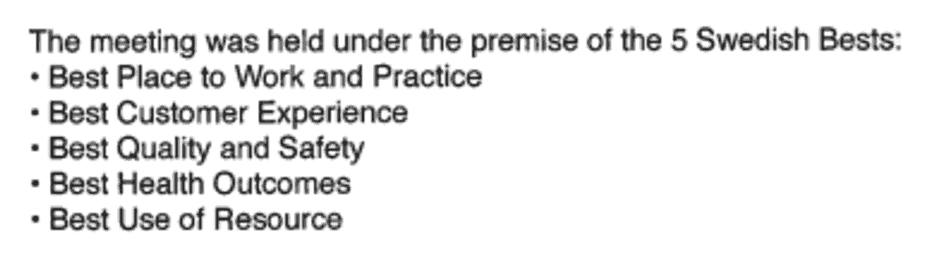
The investigation and the meeting minutes seem to suggest those “Bests” or values aren't always being lived up to.
The CEO, Armada, stated:
“…patient safety and quality are our first priority.”
Yup, they alway SAY that, as I've blogged about before:
The key is translating that goal into daily practice, as I also wrote about here:
What do you think about any of this? In the grand scheme of things, using the word “factory” is probably the least important issue.
What do you think? Please scroll down (or click) to post a comment. Or please share the post with your thoughts on LinkedIn – and follow me or connect with me there.
Did you like this post? Make sure you don't miss a post or podcast — Subscribe to get notified about posts via email daily or weekly.
Check out my latest book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation:








Mark,
Great point about the clinical service lines.
I learned from a very renown Orthopaedic group how important is is to establish a focused factory in a service line. The key to this orthopedic focused factory was that it should be grounded in evidenced-based practice.
I think Regina Hertzlinger, a prominent healthcare researcher from Harvard says it best!
http://www.medpagetoday.com/meetingcoverage/aapm/25627
It might be surprising, but as a patient, I wouldn’t want to hear the term “focused factory” in healthcare. I understand the principle from manufacturing, but I wouldn’t want it called that in healthcare.
For similar reasons, I don’t like the name Virginia Mason Production System (the “production” part). That’s always struck me as odd and inappropriate. Sure, learn from Lean and Toyota, but don’t call it “production.”
A British hospital was calling it the “Bolton Improving Care System.” ThedaCare had been using the term “ThedaCare Improvement System.”
I think language does matter…
Mark,
Good article. Most of what is expressed speaks more to a poor safety culture at Swedish and instead a culture of fear. Not uncommon in the health care sector, sadly.
Quality vs. Quantity in healthcare is a false choice. There’s a reason that US News added procedure volume to its physician profiles last year. There is a strong correlation between the number of procedures a physician or hospital has performed and clinical outcomes. Shouldice Hospital is a factory in virtually every way when it comes to hernia surgeries. But it also gets the best outcomes with the lowest infection rates. Their focus also allows them well-defined standard work and amazing OR turnaround times. If I needed hernia repair, a laparoscopic appendectomy, or any other frequently-performed surgery, I want to go to a “factory” that performs those all day every day. More efficient and better outcomes.
I agree that quantity and quality SHOULD correlate. This happens with good operations management practices, whether that’s Lean, checklists, etc. and the right culture.
Clearly, that wasn’t happening at Swedish, if more volume meant worse outcomes.
It doesn’t sound like Lean was even on the radar in the surgical department at Swedish. There’s nothing Lean in that Seattle Times story.
That’s surprising considering that Seattle is a hot spot for Lean healthcare, including Virginia Mason Medical Center, Seattle Children’s Hospital, and others.
Swedish vs Virginia Mason is actually an interesting comparison. About the same payor mix, but per HealthGrades and Definitive, VM doesn’t actually have consistently better outcomes. VM has worse outcomes for gyno, ortho, appendectomy, and other specialties. Better in bariatric and cardiac, but it’s largely a wash overall. Even their HCAHPS are reasonably close (81% overall satisfied with VM vs. 78% overall satisfied at Swedish).
Hi,
I think both Quality and Quantity are important, especially in hospitals.
A lot of people need care and i am sure that there are a lot of cases that surgeons need to work on. Unfortunately, the solution is not to disregard some patients due to maintaining the quality of the work. Nor is it taking on more patients to increase the quantity.
Its the surgeons job to help patients, its the hospitals managements job to figure out the numbers. Maybe top management should try and apply TQM to their hospital to maximize the quality of their services for their patients.
What do you think?
Of course both are important. With Lean, quality and quantity can go hand in hand, if we’re reducing waste and engaging and respecting people.
We need to meet legitimate patient demand. The Seattle Times article raises some accusations that some of the work being done went beyond patient needs. That’s a different issue. Lean would say to do what the patient needs, even if that means less money for you, the surgeon or hospital.
Top management needs to be involved in changing the culture so people can improve quality and quantity (to meet real needs) at the same time.
Update on the Swedish aspect of this post:
Swedish Health largely bans overlapping surgeries