I was planning on easing into the holidays, staying safe and healthy at home, trying to be thankful and appreciative for all that I have… and then this article ran across my radar via a Google Alert for the phrase “lean hospitals.”:
HOSPITAL CEOS HAVE GOTTEN RICH CUTTING STAFF AND SUPPLIES. NOW THEY'RE NOT READY FOR THE NEXT WAVE.
Why do I care? Well, the article bashes Lean… so that's my interest, but first, the article starts:
“IN 2006, Montefiore Medical Center in the Bronx had healthier patients, just enough nursing staff to take care of them, and a CEO who was earning $2 million a year, a senior nurse and union leader told The Intercept. Fifteen years later, its patients are sicker than ever before, its staffing levels are inadequate, and, as of 2018, its new CEO is earning $13 million per year.”
That's a fair question… should the new CEO be earning 5.5x what a CEO at that same system earned just 14 years ago? The conversation about “excessive CEO pay” has been going on for decades and it probably pre-dates the origins of the term “Lean Production” in the late 1980s.
But, things go downhill with the first use of the word “leaner” — using “lean” in a way that's not the capital-L “Lean” methodology that we know and practice:
“The nonprofit hospital, like hundreds of others across the nation, has been cutting costs, progressively going leaner on staffing and supplies over the years.”
Lean (in the sense of the capital-L methodology) doesn't mean LESS… it means having the right number of people and the right resources in place. It's about effectiveness, not about being cheap.
I think there is an expression that goes back to Drucker or Deming or somebody like that… “any fool can cut costs.”
Maybe they didn't say it, but I agree with the statement and the sentiment. Too many healthcare executives have been foolishly slashing staffing levels and inventory levels for a long time. They've made those mistakes without Lean. That's just called “healthcare cost cutting” and it can really dysfunctional. “Any fool” can cut costs in a way that, unfortunately, harms safety, quality, and morale. Some attempts at “cost cutting” end up costing the organization MORE over time.
If executives have a mindset of “cost cutting first,” then there's a risk that they learn a new method like Lean (or mis-learn it) and then use it for cost cost cost.
There are, sadly, consultants out there who will claim to be Lean experts, but their approach is all cost cost cost (as I've written about and complained about before).
That's not Lean, to focus primarily on cost or ONLY on cost. I haven't trotted out this acronym in a while, as I'm hesitant to use it, but it would be “L.A.M.E.” (not Lean) to focus primarily on cost.
Our Lean origins in Toyota would have us focus on Safety, Quality, Access, Cost, and Morale. Reducing cost is the END RESULT of first improving safety, quality, and access. We aim to improve morale by making sure they are no longer overburdened (again, a long-standing problem in healthcare) as Lean aims to make work EASIER for everybody involved, not harder.
Lean means having the RIGHT amount of staff, the RIGHT amount of inventory. If you've got shortages of either, it's really unfair to blame Lean. These problems have been in healthcare for a really long time — they pre-date Lean, they weren't caused by Lean. Some organizations (but not enough) have solved some of these problems… using Lean.
Leave My Name Out of It!
I'll admit to being fired up and I'm writing this with my “reptile brain” as I'm really angry that I was mentioned in this hit piece:
“The concept of lean hospitals was developed by management consultant Mark Graban in 2009, but business practices imported from manufacturing based on lean staffing began to be introduced in health care starting in the early '90s.”
For one, that's factually incorrect — I did not “develop” the concept of Lean hospitals. My book, Lean Hospitals: Improving Quaity, Patient Safety, and Employee Engagement was not even the first book on the subject.
Secondly, I'm upset that the “journalist” here didn't even bother to contact me for my perspective. I'm obnoxiously easy to find online and I do respond to reporters who reach out (and was quoted in a positive piece about Lean in the New York Times about Lean at Seattle Children's back in 2010).
Update: He did reach out for comment, which is now part of that piece… more details below.
Update: He's not a journalist, he's a writer who works for a nurses' union, per his bio. That should have been disclosed more clearly. It's an “opinion” piece that should be labeled as such.
If you're going to name me and indirectly blame me for bad healthcare management… that's awful. Leave my name out of it. Or, ask me for input if you're going to drag my name through the mud.
Let's Hear BOTH Sides
I'm all for reporting that shares both sides of a story. I once talked to a reporter who was very concerned that her editor wouldn't print her piece because everybody who was quoted was glowingly POSITIVE about Lean in healthcare. I even went out of my way to try to make introductions to one state's Nurses Association (Union) who I knew would bad mouth Lean.
But, when a union is bashing Lean, I've found that there is generally a really bad pre-existing relationship with management teams who might be seen as untrustworthy. So, if management is saying “Lean is good,” some unions will have the understandable knee-jerk response of “No, Lean must be bad.”
The the article that triggered this blog post is shockingly (and unfairly) one-sided.
The website, “The Intercept” claims to be an “award-winning news organization,” but it seems like they've published a union hit piece written by a union man. The author, Matthew Cunningham-Cook's Twitter profile says he is a “990 knower for a fighting labor union.” Objective journalism? That's no more objective as I could claim to be as a consultant in this field. BTW, Form 990 is a public disclosure that must be made by non-profit organizations.
Update: The writer did reach out for comment, which is now included in the article.
“Graban said that some executives have drawn the wrong lessons from the management practice. “It's unfortunate, if not harmful, when hospital executives misunderstand Lean to mean cost cutting, working harder, or not having enough supplies,” he said. “Lean, with its origins at Toyota, provides a management system and improvement method that focuses on first improving safety, quality, and access to care — and there are many published journal articles that document this. Lean aims to reduce the overburden on workers by improving the way work is done. A true ‘just in time' system is designed to have the right number of people and supplies and medications. Lean organizations don't boost the bottom line at the expense of employees, with UMass Memorial Health as a noteworthy example of a system that had a ‘no furloughs, no layoffs' commitment even during this pandemic. “
Lean Organizations Fight Against Overburden and Shortages of Supplies!
Anyway, back to the article… it describes a problem that I agree is a a problem:
“The nurse, Karine Raymond, has provided care at the facility for 27 years. In the second wave of Covid-19, as in the first, she and her colleagues are taking care of double the patients that they typically do.”
Being overburdened is bad. Lean aims to reduce overburden, as I wrote in Lean Hospitals:
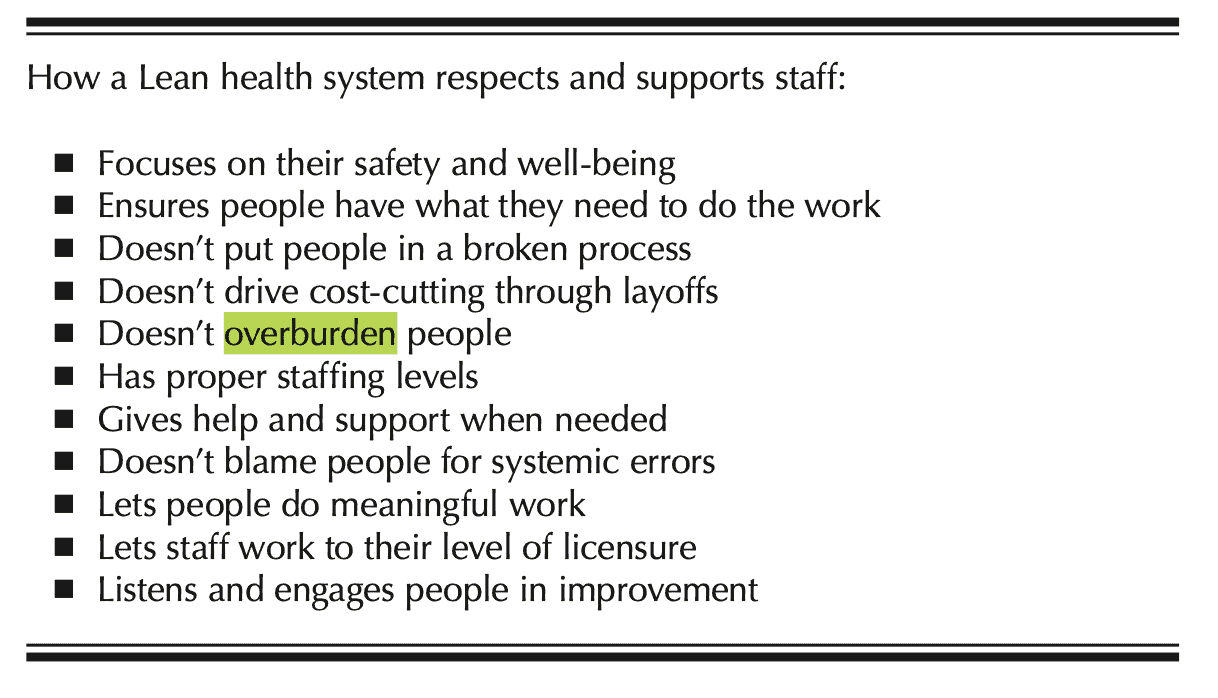
I also wrote (the word “overburden” appears 10 times):
“Japanese not only has a word for waste (muda), but also has specific words that describe overwork (muri) and uneven workloads (mura). Having respect for people means we do not allow our employees to be over-worked or overburdened. Lean is not about pushing people to work too quickly or to be in two places at the same time.”
Again, overburden is BAD. Dealing with the unprecedented workloads in a Covid era is a huge challenge, but a truly Lean hospital would have enough employees (and enough equipment and enough medication) to meet patient needs without overburdening people.
A nursing professor says:
“Even before the pandemic hit us so hard hospitals were using a policy called ‘Lean,' which is just-in-time staffing and supplies,” said Linda Aiken, a professor of nursing at the University of Pennsylvania who has long studied the relationship between nurse staffing and patient care.
I'm not sure how she is qualified to be quoted as an expert in Lean.
As I blogged about earlier this year, “just in time” doesn't mean “low inventory” and it especially doesn't mean “not enough.” A truly just-in-time system requires a supply chain that's designed to be flexible. When corporations (including non-profit healthcare systems) insist on buying the cheapest components, that drives production to China — and a long supply chain like that can't be a responsive supply chain.
Effective “just in time” requires local suppliers. I think the unions and I would be in agreement that more American manufacturing would be a good thing for many reasons.
Then there is the paragraph that mentions me:
“The concept of lean hospitals was developed by management consultant Mark Graban in 2009, but business practices imported from manufacturing based on lean staffing began to be introduced in health care starting in the early '90s. “All of our research shows those policies were a failure well before Covid and now they are a disaster during this national emergency,” said Aiken.”
“All of our research” meaning whose research??? There is PLENTY of published research out there that's positive about Lean, that Lean is not a failure in normal times. A truly objective journalist would have sought that out.
And to say “lean staffing” as to imply “not enough” is NOT what Lean is about. Again, he could have asked me or looked at my book.
Being understaffed is a disaster… and hospitals have, again, been doing that before Lean and without Lean.
Another union leader piles on in this unbalanced piece:
“Bonnie Castillo, executive director of National Nurses United, the largest union of registered nurses in the U.S., lambasted “Lean” in a statement at the beginning of December, saying, “Lean industry practices slashed preparedness. They treat safe staffing and needed supplies as a drag on budget goals and profit margins, rather than the prerequisite for a humane, fully prepared patient-oriented health care system.”
Who in their right mind, a Lean advocate or not, would be in favor or less preparedness for a pandemic? That insulting. A Lean hospital focuses on “humane and fully prepared patient-oriented” care, as a Dutch hospital demonstrated years ago as Lean being what they called their “Loving Care” system.
The union says:
“Lean policy has had concrete results on the ground. “During the current surge, nurses are seeing patients die who could have been saved, if they had the proper staffing and supplies,” National Nurses United said in a recent statement.”
Again, being understaffed and being short of supplies, like PPE, is NOT Lean. Dr. Eric Dickson, CEO of UMass Memorial Health, had a “no furloughs, no layoffs” policy during the pandemic (driven by Lean thinking and his advisor who is a former Toyota leaders). Dr. Dickson invested in their people and in process improvement… and he said the hospital is STRONGER as a result. We talk about that in this podcast. That's what Lean is all about. Lean is not irresponsible and dysfunctional cost cutting. Learn more in my podcast with Dr. Dickson.
As I wrote about in Lean Hospitals:
“The [Lean] kanban approach is sometimes mistakenly thought of as a system that just focuses on low inventory levels when its goals are actually to support the patients and the employees by ensuring needed supplies are in the right place, in the right quantity, and at the right time and to ensure the availability of material with the lowest required inventory levels. Kanban systems typically have fewer stockouts and better availability of materials than traditional materials management methods.”
The article then returns to the issue of CEO compensation and tax benefits. To me, that's a different discussion. It's worth having, but not if you're going to also blame Lean for everything that's currently messed up in healthcare.
The shortages of PPE are heartbreaking. That said, I bet there is ZERO correlation between Lean practices at a given hospital (or lack thereof) and supply shortages. These are global supply chain issues… “Lean” hospitals face shortages, as do hospitals that have done nothing to embrace Lean.
I'll stop ranting about the slanted and biased blaming of Lean for problems that have existed in healthcare for decades.
Again, the author didn't reach out to me. The article didn't quote any healthcare executives. This wasn't “journalism” — it was an agenda-driven hit piece driven by union leaders and academics who are probably sympathetic. That's shameful.
As an ironic aside, I'll be labeled a “union basher” as a result of this piece (and others). The Texas Hospital Association had a communications director accuse me of being a “union organizer” years ago when I spoke up about problems at Dallas hospitals during the Ebola era. Go figure.
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s work together to build a culture of continuous improvement and psychological safety. If you're a leader looking to create lasting change—not just projects—I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s start a conversation.







![When Was the Last Time a Leader Around You Admitted They Were Wrong? [Poll]](https://www.leanblog.org/wp-content/uploads/2025/07/Lean-Blog-Post-Cover-Image-2025-07-01T212509.843-100x75.jpg)

Mark, thank you for your response to this article. This is not the first time I have heard Lean being used as an excuse, or cause, of low inventory or staff, however it is the first time I have seen such complete ignorance and disregard for using people’s expertise (yours) against them. I’m sorry for that.
I saw that the writer, in his Twitter feed, shared an article from “Labor Notes” (at least that’s obviously a union publication) that rips Toyota.
https://www.labornotes.org/blogs/2010/03/toyota-and-myth-quality
So, he’s got that single perspective drilled into his head — lean bad! Toyota bad! Management bad! The one article he tweeted rips Toyota for closing the NUMMI plant. Um, that really closed because GM pulled out of the partnership. That plant only reopened in the 80s because of Toyota. And, the union will never admit that Toyota didn’t lay full time employees off during the great recession and other downturns… like I said, there’s an agenda and I’m not convinced that agenda is about making healthcare better.
Other perspectives on Toyota NOT laying off people:
https://www.linkedin.com/pulse/main-lesson-businesses-hospitals-can-learn-from-toyota-mark-graban/
https://www.leanblog.org/2016/02/is-this-the-one-question-that-determines-if-youre-truly-a-lean-thinking-hospital/
https://www.leanblog.org/2016/05/again-toyota-chooses-to-pay-workers-when-production-is-down/
And an article about another CEO and his no layoffs philosophy:
https://www.leanblog.org/2015/04/the-scripps-health-ceo-is-right-about-no-layoffs-policies/
In some ways it could be read as a good thing. A sign that Lean has taken hold significantly enough in the Healthcare industry to be seen as a threat in some way. Mis-categorizing your statements and writing is commonplace in a hit piece. Maybe there are now further conversations to be had and work to be done with the groups feeling threatened?
I think there are MANY conversations that are needed to restore trust between management and healthcare professionals. Without trust, there’s no hope for conversations (and action) related to Lean.
You are covering a major frustration for someone who has spent years helping healthcare become more Lean (with the capital L).
I am not a surgeon. If I perform surgery and skip important concepts or use poor surgical methods and practices it does not mean that surgery as a concept is bad. It means the implementor (the untrained surgeon) needs improvement.
Why are hospitals failing to see that when they misuse Lean principles and their transformation fails it is due to failure to understand and practice important principles?
Now that this is off your chest, have a great holiday!
Thanks for commenting, Steve.
I don’t have a simple answer to your question… “why are hospitals failing to see…?” Cognitive biases in leaders… ego… an unwillingness to take responsibility for “failure” or to learn from it quickly… people are complicated!
Thanks for sharing Mark. I appreciate you not letting this one slide through unchecked. The Union should be the first to embrace all Lean has to offer. If they were to get behind Lean we would be much further along in reaching its full potential with obvious benefits to patients, employees, and the organization. Curious if you have read Bob Emiliani’s book “the triumph of classical management over lean management – how tradition prevails and what to do about it”? It seems to address many of the same issues raised here. I would be interested in your take on it. Hope all is well, it has been too long!
Commenting late on this, but speaking as someone who’s been both in the front-line worker seat and the “transformation leader” seat, I think this defensive “no true Scotsman” approach isn’t going to do anyone any favors. There *are* bad actors in this industry using “lean” as an excuse for understaffing, overworking, layoffs, and leaving no room in front-line workers’ schedules for the transformative work that inspires joy and ownership. Rather than a knee-jerk “you’re being unfair,” I think we have some listening to do – why is this the perception? How can we challenge these so-called “lean leaders” and stand in solidarity with the rest of our workforce? We all have the same goals – an efficient, working healthcare system, with time for improvement, leisure, and joy in work – so there’s no need to be defensive.
Thanks for reading and commenting, Milo.
I guess I was expressing my frustration not only with the writer (at least he took time to hear my side of this story) but also my annoyance at the “bad actors” as you described them.
There is something to be said for understanding why the perception exists — the word “Lean” isn’t ideal in a number of ways and the bad actors give Lean a bad name.
But I also think some writers have an agenda to paint everything done by corporations (even big non-profit healthcare corporations) and executives as bad and greed driven.