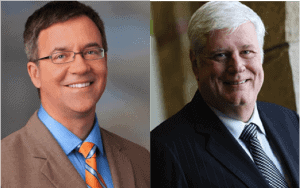
My guests for episode #226 are Steve Hoeft and Dr. Robert (Bob) Pryor from Baylor Scott & White Health in Texas.
Bob serves as President, Chief Operating Officer and Chief Medical Officer for the system and was formerly CEO of Scott & White Health before their merger with Baylor Health Care System. Steve is the Chief of Operations Excellence for the system.
They are co-authors of a recently released book that I think is outstanding: The Power of Ideas to Transform Healthcare: Engaging Staff by Building Daily Lean Management Systems.
Steve is also previously author of another book I really like, Stories from My Sensei: Two Decades of Lessons Learned Implementing Toyota-Style Systems.
I'm sure you'll enjoy the podcast, as they combine the perspectives of an industrial engineer and Toyota-influenced automotive guy (Steve) and a pediatrician and physician executive (Bob). They share a passion for healthcare improvement AND a belief that we need to respect and engage everybody who works in healthcare as a way to better serve patients.
Streaming Player

In the podcast, we discuss topics including:
- Can you tell us about how legacy Scott & White got started with Lean? What was Bob's role as CEO of the system?
- Can you give an overview of the daily huddle system and how that cascades through the organization?
- What are some of your greatest success stories, in terms of results?
- How did you know when the culture was really changing? That you're shifting from a culture of blame to a culture of safety?
- Has it helped to bring in other Toyota or Toyota-trained people?
- Now that Scott & White merged with Baylor to become Baylor Scott & White, what have been some of the strengths and opportunities as you combine organizations and cultures? Can you speak to any differences in the Lean approach in both organizations?
For a link to this episode, refer people to www.leanblog.org/226.
For earlier episodes of my podcast, visit the main Podcast page, which includes information on how to subscribe via RSS, through Android apps, or via Apple Podcasts. You can also subscribe and listen via Stitcher.
Transcript:
Mark Graban: Hi, this is Mark Graban. Welcome to episode 226 of the podcast. It is July 29, 2015. My guests today are Steve Hoeft and Dr. Robert Pryor, or Bob, as he prefers to be called, from the Baylor Scott & White Health system in North Texas.1 Bob serves as the President, Chief Operating Officer, and Chief Medical Officer for the system and was previously CEO of Scott & White Health before their merger with Baylor about two years ago.2
Steve is the Chief of Operations Excellence for the system and they're both co-authors of a recently released book that I think is just really outstanding.3 The book is titled The Power of Ideas to Transform Healthcare: Engaging Staff by Building Daily Lean Management Systems. Now Steve is also previously the author of another book, Stories from My Two Decades of Lessons Learned Implementing Toyota Style Systems. Both of those books are published by the publisher that's released both of my books, CRC Press or Productivity Press, which is a part of CRC. I'm sure you'll enjoy the podcast as Steve and Bob combine the perspectives of an industrial engineer and a Toyota-influenced automotive guy, Steve, and a pediatrician and physician executive, Bob. They share a passion for healthcare improvement and a belief that we need to respect and engage everybody who works in healthcare as a way to better serve patients and I guess I would also add to perform better as a healthcare organization. So I think you'll really enjoy the discussion. I've been fortunate to be able to visit with them a couple of times in person at their Gemba, if you will, at the hospitals in Round Rock and in Temple, Texas. And now they've got the broader Baylor Scott & White system that includes the Dallas Fort Worth area. If you want to see links to the book or more information about either of them, you can go to leanblog.org/226.4
Well, Steve and Bob, thanks so much for being guests on the podcast today.
Steve Hoeft: You're very welcome.
Bob Pryor: Yes, thank you for having us.
Mark Graban: So Bob, if you can get us started, I'd really be curious to hear about how Legacy Scott & White originally got started with Lean. And if you could sort of also talk about your role when you were the CEO of the system.
Bob Pryor: Well, thanks. It actually started before I was the CEO. I had moved to Temple, Texas and had been on the West Coast in the Phoenix area and came back and found that I was to be in operations. And coming from a physician standpoint to going into operations, I was searching for the right way to bring a people solution to our operations. I saw several problems within Legacy Scott & White. Number one was I had no idea how communication got from where the ideas were formulated up in the executive suite down to where the people who were really important, who were doing the work, knew exactly how they fit in and what to do. Also, there was no way to get communication back from these very important people that were the sharp end of our patient care to get communication back up to where I knew what was going on. And as I was searching, the Lean tool that I had learned in business school kind of kept coming back as to saying, “Now we only spent about a half a day on this in operations management and business school, but this seemed to be the solution I was looking for to how to get a people solution into operations so that everybody was aligned and everybody came to work every day and knew what they had to do so the organization could push forward.” Also, since healthcare was changing so rapidly, how could we change our focus in a speed that was anywhere approximated the speed in which we needed to change as external forces were changing healthcare? So we decided to get started on a Lean journey because that seemed to solve all the problems that we were facing.
Mark Graban: And what was the time frame for you discovering or finding that Lean was going to be your approach?
Bob Pryor: Well, first I had to learn a whole lot more about it. As I said, I had about a half a day in operations management at business school. So I started educating myself, took advantage of some courses and read a lot on my own and validated within myself that this was the right way to go. Then I started broadening the scope of the people that were involved in the transformation. One of the things in healthcare is that every new idea is met with incredible skepticism, especially among physicians. They're very skeptical about any change that's taking place. And certainly our older employees that have been through many, many new young leaders that come in and there's a flash in the pan new idea about how we're going to change the organization for the better. And many of them sit back and say, “Well, I don't really have to learn this. All I have to do is outlast you. You're going to last about two years, young man, and two years from now we'll be doing something else. So I don't really need to learn this.” So we started expanding the scope and involving the leadership and then we started involving people at the front line. And I had this idea that, a very naive idea that all I had to do is to bring in a teacher and teach everybody the tools and suddenly everybody would be happy and this would be going. I met Steve Hoeft. And I actually asked Steve one day, I said, “Steve, what do you think the chances of us putting Lean together by teaching at least to a tipping point in the organization so that everybody understood these tools and everybody was getting ready to go?” And he looked at me and said, “Bob, that would be zero.” And that was incredibly true. But anyway, that's how we started the journey. But then of course, from that start, we've had a very purposeful, driven journey into Lean since then.
Mark Graban: Yeah. And so that's a good transition to hearing Steve's perspective on those initial discussions and how Steve got to be involved. But first off, just for the listeners, what was the time frame? What was the year when you were kind of starting with that?
Bob Pryor: That would have been about eight years ago.
Mark Graban: Okay.
Steve Hoeft: Late 2007. And that's when Bob and I met.
Mark Graban: So Steve, talk a little bit about your background and how some of those conversations came to be leading to you getting directly involved with Scott & White and the Lean journey.
Steve Hoeft: Yeah, and I'll skip that whole earlier days that the Stories from My Sensei book really covers that well. But I wanted to focus on Bob too. Bob and I met during a university-based training class I was teaching. And he made that statement that maybe we can just do training for a while and maybe that'll create a tipping point. And I said, “That's kind of crazy. If you don't immediately, it's not going to work.” Bob had heard from every consultant that, “Oh, sure, Bob, we'll take your money, we'll make belts for you, we'll do training for you.” I think I was the only person gutsy enough to say, “That's just stupid, boss. What does that mean? How are you going to do that?” I like the fact that Bob was a CEO MD. Think about that. How many times, Mark, you and I have seen that's like almost the magic success factor? You have a major. Whoever is doing this really well, it seems to be somebody with that deep clinical knowledge who is also a leader and is the CEO. When the CEO gets it, the organization gets it. So I was coaching about 30 different large health systems, but Scott & White was my favorite. And it was simple. It wasn't just Bob. There seemed to be at little Scott & White in Central Texas a real desperation. They wanted to bend the cost curve. They wanted to get all staff engaged. They wanted to do population health. They needed to get all of their costs and length of stay less than Medicare, all while they were growing exponentially. So I just fell in love with Scott & White. It was just a matter of time before I was consulting, but just a matter of time before Bob said, “Steve, stop talking about this crap and come down here and actually do something. You're swooping in once a month and come down here and help me turn this thing. Let's get a transformation.” And the rest is history. That was almost seven years ago. And we really, the people here have done some good.
Mark Graban: Now, a couple of minutes ago, and I think the sound cut out, unfortunately, when you were talking about this idea of can you just do training? You said you also need to… Were you saying you also need to go and do something? What was that statement you made?
Steve Hoeft: Yes. The reason why I told Bob you had a 0% chance of success if you do training, is that training from a conference room with everybody eating donuts, by the end of that time, the only thing you've really accomplished is people know how to eat donuts. I told him, “I refuse to be involved in anything if there's leaders in that room learning, they will immediately apply it. We're not going to count the dead bodies in training class. We're only going to count whether or not they immediately go out and apply this on some sort of transformation activity.” So that's the same thing we have true here even today at Baylor Scott & White Health. They do not go to training. They get sent by their leaders to accomplish something. They're going to build something immediately coming out of that training class or they won't go.
Mark Graban: Yeah, well, I think we see a lot of health systems that fall into that trap. They do lots of training, whether they're certifying people as belts or not. I mean, it's a shame when I see sometimes people get their interest piqued, they get excited from what they hear in the training. But then the culture and the environment and the lack of a daily lean management system really gets in the way of them going and doing anything. So I don't know why you would frustrate people like that by training them and not letting them take action as people in healthcare so desperately want to do. Bob, let me ask a follow up. Steve was talking about, I think when I said, the desperation to bend the cost curve and improve. I mean, at a starting point, Scott & White, I think it's fair to say, was a pretty highly regarded health system. So it seems like as an outsider, it was by no means a complete turnaround scenario. Would you describe it as trying to go from good to great or how would you describe where that drive came from?
Bob Pryor: You know, I think “good to great” is a good place to start because we were for 115 years an isolated island in central Texas and we were a closed model with physicians who came to work every day to do the best they could. But we weren't building the processes around these physicians that would get us to the point where every day we could improve. Some days a lot, some days a little, but every day improve. So as we started moving forward, we immediately involved physicians and we didn't let the physicians just be passive observers. The physicians were involved. And it's amazing that now the physicians, part of their compensation plan, fast forward to today is, do they huddle or do they not huddle? So that's actually part of the physician comp plan at Legacy Scott & White Clinic.
So as we started moving forward, it was important to me, as you said, and I can't overstate this, the culture had to change. It had to be a change in the culture. It had to be a change so that everybody felt every day this direct line of sight between what the organization wanted to accomplish and how the people were going to accomplish it. And sometimes I see that that's what's lacking in strategy. I mean, one of the things that I have realized is that every health system in the country probably has the same strategy, or at least 90% overlap of the strategy. But what a lot of organizations don't have is how do you take that strategy and convert it into action at the front lines? And that's a cultural change. And cultures change slowly because it's culture, because it's the way that we take all of our norms and try to produce an outcome. When you start changing those norms, it has to be organic, it has to come from the ground up.
Mark Graban: I want to come back to some questions about culture in a few minutes, but maybe first back over to Steve. As you mentioned, the book you'd written previously, Stories from My Sensei, which I really enjoyed and recommend for people to really it's a fun read. Can you talk about the story of your new book, The Power of Ideas to Transform Healthcare? How did that book come to be? How would you describe the focus of the book and how you got Bob involved as well?
Steve Hoeft: Yeah, how it came to be is, the one-word answer, it was really need. There really is a lack of specific how-to books in healthcare. And Mark, you know you've written two good ones but think about that. There's not like, “Here's how you do value stream mapping, here's how you do Kaizen events, here's a good way to do a whole hospital-wide assessment.” You know, they just, they exist for manufacturing, even for some service, but they just don't make it. And I think that's why your role has been so significant in trying to promote this within the healthcare industry.
So we had so many books we are using as a pre-read. We get away with minimum time in the training classroom formal because we do so much with the application but also because we require our leaders to do quite a bit of pre-reading. We can't just yak at them. So we're using many different books as pre-reads for our classes. One of them for our daily lean management system building was Creating a Lean Culture by David Mann. And David, he was very kind to write our foreword, some very positive words. He loved what he saw down here, but his book was at least in earlier versions so specific towards Steelcase and the examples that were there. We needed pre-reads, we needed the go-deeper books to go alongside our very brief books. So Bob and I, we really wrote the book to be the pre-read and kind of the go-deeper book for our own courses and we realized that we're sharing right where we're at in a really raw way with every healthcare system, including the competition. And this is the right thing to do. This is exactly what Toyota would do.
Mark Graban: And yeah, I mean, I would agree. I think David's book is excellent. Even that first edition that was, I think, written about manufacturing experience I gave and recommended that healthcare leaders buy that book. And people found that really helpful in terms of understanding, at least generally, what is meant by the components of a daily lean management system. And that's a big part of what you focus on in the book. So within that, I'd be curious to hear thoughts from either of you about your daily huddle system. I've been able to observe some of that huddles that were taking place at different levels and how that fits into the broader lean management system. Bob, would you maybe like to address that first from your perspective?
Bob Pryor: Well, one of the things I can say is that huddles have been a transformative stage in our journey. And it's one of the things that as Steve would sit back and watch me struggle and watch me sweat and he would just allow me to learn a little bit more. And one day I forgot what the topic was. And Steve said, “Oh, yeah, Bob, I haven't taught you about huddles yet.” And then when he started describing huddles, it made all the sense in the world that by using the huddles, we not only harness the ideas and the power of everyone who works in our organization, but when you put that in with the cascading of the goals and you align that, now everyone in the organization understands what they need to do for us to move forward. And the huddles were transformational. The other part about huddles is that as I encourage the senior leaders to go out and see on the shop floor, the huddles make it very easy for them to be very efficient. And they can go and go to several huddles in a very short period of time and cover a lot of ground and ask the appropriate questions. And that does several things. Number one is it shows the frontline people that the executives really care about what's going on and about them as a person. And the other thing it does is that it continually realigns. And then the third thing it does is it allows for spread. This is one of the ways that you can spread the ideas rapidly in the organization.
Mark Graban: Yeah, I was impressed when I got to see those huddles that were taking place at different levels. It wasn't, I guess it was impressive that there was a pretty standardized approach to the huddles. But I think the most important thing was the sense of alignment in terms of what priorities were about, what to bring up, what to discuss and how information was flowing up from the frontline focused huddles all the way up to the executive team, and that the executive team was huddling and that information could then cascade back down. That was really good to see. Steve, maybe a question for you, just more generally about huddles and how you've coached people on this. I think huddles is one of those practices where people say, “Oh, okay, yeah, that seems simple.” And they sort of try to copy what another organization did in a rote way. And then unfortunately, what develops is people are just sort of checking the box. If you ask, “Why are you huddling?” They might say, “Well, because they told us to huddle.” And there's not the same spirit involved in the huddle. Do you have any thoughts on that, of how to make sure those huddles are not just a check the box activity, that they're useful to the organization and everyone involved?
Steve Hoeft: Yeah. If I had a nickel for every time in healthcare I've heard people say, “Ah, we already huddle.” And maybe that's been the power of why it's been so quick. I mean, Bob's talked about, in some cases, we've turned this ship, a big ship in two weeks, we can be heading off and taking new ground in a new, different direction, whether it's access or population health. But I think the key and the reason why that it's different and maybe Mark, what you saw when you first came down here about the linkage and all, we're using Hoshin Kanri just to use that concept to link every single person so that they can see how they fit into the vision, mission, and value of Baylor Scott & White Health. So people really do feel like they're not just huddling over quality work life issues. They're huddling over meaningful stuff. So that was very important that we did differently. But maybe the biggest key is leadership. A top leader is trained first. We won't do this unless the top leader is trained first. That leader doesn't tell her staff, “You go huddle.” She says, “Come to see my huddle, and then I want you to make yours better.”5 They lead by example in this case. So we did not start at the bottom with the troops. We started at the top and of course we kind of met in the middle here. But each leader has to start their own huddle and they have to sponsor a tier one direct performer huddle. And that's where everything, remember there's no training class. They come on the next day after the end of their class, they're expected to huddle and they're going to be bringing their staff members to their side of the huddle.
So flipping it around and saying, “Leaders, you have a job. It is management's job to build the systems by which workers can check whether ideas are working.”6 Our huddle processes, because everybody huddles, we've actually had to start calling them idea huddles because the whole purpose of this is to bring forward a base-hit idea and while people are working, try it out. Bob started to say that we hit the exclusive accelerator point. How many projects can a health system do in a year? 10. And 10 or 12 people are on each project. What did the other 12,000 employees do? How are we going to get them involved? And yet every one of them have ideas. So Bob and I realized this at one point. It was a Toyota tour, and every one of those Toyota workers, we happened to go to Kentucky, although San Antonio, Mark, is better and more powerful for this picture. But every employee, every week, every month, they're coming up and implementing ideas. And Bob's like, “We're just as smart as them.” But we realized we weren't even asking, we didn't even ask our staff for their ideas. And we had these things. All healthcare people huddle. So during the huddle, why don't we pick one metric, point with the finger, make sure that they're daily or weekly measured. That's a key to this thing too, and meaningful. “Here's where we're at, here's where we need to go.” Have the leaders ask, “What could we try today while we're working? What could we try today together to try to close that gap?” And the answer to that astounds Bob every day is that daily innovation, that healthcare workers are great at this.
And if I could just say one thing, Mark, this is the passion part. Bob and I watch people physically, visibly change. Something changes inside of a person when their boss says, “I don't know what else to try. Maybe it's falls, right? This could be our mother, this could be our grandmother, our neighbor. I don't know what else to try. We've tried A, B, and C so far this month.” And they look at the team and say, “I don't know what to try, but I believe you do. What could we try together as a team while we're working together to budge this number?” And people brainstorm and somebody comes up with a great idea, they always do. And when it works and the boss says thank you, they go home at night and they tell their kids, “Kids, if I wasn't at Baylor Scott & White, it'd be going… I'm single-handedly meeting all my department's goals.” I don't care if you call it Lean or daily Lean or huddle, it doesn't matter what you call it, you can't take it away from them. They're going to tell kids, “You know what, I'm going to give them another idea next week. I really like what I do.” So we've watched that click, Bob, just the second ever huddle up at our new site in Irving and they were so excited. It's the second ever and an idea came up right there while we were filming with Bob and Bob was watching that engagement, that excitement in their eyes again. And we're not going to do it any other way.
Mark Graban: I want to ask Bob about some of the results or measures. Obviously there's a lot of focus on systems and process and huddles. But like you said, you're trying to close gaps. You're trying to do things like reduce falls and improve care. So Bob, what are some of the most noteworthy successes that Scott & White can hang your hats on in terms of results and measures? What's the impact?
Bob Pryor: Sure, thanks. We could talk about macro measures or micro measures. One of the measures that I'm most proud of is that when we first started the huddles at the sharp end of care, we looked at employee engagement and those groups that were having daily huddles knocked the top off the employee engagement survey. We had been trying to get employee engagement for years and weren't making any progress. We even had somebody come in and they gave us an off-the-shelf plan to improve employee engagement. It didn't work. But the second that effective huddle started, employee engagement just went off the top of the scale, and then this produces much more satisfied employees. So what followed from that was patient satisfaction went way up. So if you look at the groups that are huddling, and you look at the group, especially that huddle, with their daily metric of patient satisfaction, now employee engagement starts, followed rapidly by incredible increases in patient satisfaction. And that actually is what I'm most proud of. We've also had other financial issues that we've solved. We've certainly cut our costs, we've become more effective, our productivity is up, morale is up. So if you look at all of the dimensions across Lean, every one of them, we're making big strides to advance. But the thing that I like the most is the fact that we've come together as a group in a way that we'd never come together before. We're actually one group now, not many different tribes. We're one group that we're all pulling the oars in the same direction. And whatever we want to do, I'm convinced that we can get it done.
Mark Graban: In a week in terms of going from idea to something being implemented, instead of having a big committee that just gets together monthly to talk about the problem.
Bob Pryor: Right, sure, it goes that way, but it also goes the other way. When we find something that's of strategic importance to our organization, we can go that way as well and parse that out so that everybody's working on it and the ideas are spreading through the Gemba walks.
Mark Graban: Yeah, well, I think that's a challenge. One of you mentioned the idea that a lot of organizations have the same strategy. I've been in organizations where frontline staff or even people within an internal lean department will challenge their executives and say, “Nobody knows what our strategy is. Nobody really knows what the most important goals are,” other than at the vague level of, “Well, we're trying to care for patients.” And so, yeah, that communication and alignment, it's still pretty rare in healthcare. Maybe you do remember back to the before situation, but that does make a big difference when organizations have that alignment. So, Bob, I wanted to ask one other question. Maybe Steve, you can jump in too. You're talking about culture, and culture is probably something that's hard to measure. You know, in the book, you talk about a topic that's really important to me, shifting from a culture of blame to a culture of safety. So I was wondering maybe, Bob, first, if you could talk about that, how do you make that culture change a reality? How do you know when the culture is changing?
Bob Pryor: Well, first of all, healthcare is kind of like what I learned in surgery. The ABCs of surgery: assess, blame, and criticize. So moving from assess, blame, and criticize to “here's an issue, and we have very, very good people working, but they're working with bad processes.” So let's design our processes so that it gives everyone a chance to succeed wildly. And when we succeed, our patients, of course, succeed. And when you really know that the culture is changing is by stories. Stories tell the culture of an organization. So when the stories start shifting from, “Well, let me tell you what's wrong in this organization.” As a matter of fact, I was in an organization the other day that was outside of healthcare, and I just happened to hear some of the employees talking, and they were saying, “Well, what do you think about those new people? Don't those new people have it all wrong?” And they spent 15 minutes while they weren't working complaining about their organization. So when the people start coming together at the front end of care and start telling stories about, “Let me tell you what we've done. Let me tell you about how we've changed the way that we work. Let me tell you how we came together.” And once you start hearing those stories, then you know that culture has changed from one of “I'm really afraid to step out of my box and speak up” to, “Let me tell you how I spoke up, and let me tell you how that changed our whole organization.” Steve mentioned the example of when I went to the second huddle this one group had, and they came up with an incredible idea of how to reduce overtime. It was an incredible idea. They put it into effect in one day and they had overtime solved. One of them who was part of the idea generation asked me. She looked at me point blank and said, “Is anybody going to know that we did this?” I said, “Absolutely, I'm going to tell everybody you did this.” And I've been telling everybody this story. But after two days of huddling, they solved a problem they've been struggling with for years. They solved it in one huddle. And not only that, but then the other thing is, I followed it with a letter to them and told them that not only did I promise you I was going to tell everybody, I have told everybody, and thank you for generating that. So that's where culture changes.
Mark Graban: Yeah. So, Steve, let me turn back to you, and I'm curious from your perspective, from your time at Toyota, you get a sense visiting Toyota, or at least within the Lean philosophy or TPS approach, that safety as a top priority is more than lip service, that it's the reality of making safety a priority, making choices that err on the side of safety. In a lot of health systems, it's easy to say, “Oh, we always make patient safety a top priority,” but that doesn't necessarily seem to play out in people's daily decisions or what the organization is allowing them to do. So I'm curious, what are some of your thoughts and perspectives about learning from Toyota, trying to change the safety culture in healthcare?
Steve Hoeft: Yeah, that's been one of, maybe the, that's really been the success story. If we were to try to pick one of the metrics, Bob and I, we kind of picked Toyota's categories of metrics to try to roll things out early on. Now we use our circle of care. The four things that we've got to get done as an organization at Baylor Scott & White. When we first got started, we thought, “It's good enough for Toyota, it's good enough for us.” SQDCM: safety, then quality, then cost, then delivery, which is sort of your timeliness and that access is part of it. And morale. It's not that morale, employee morale is the last. But of the hundred categories of metrics, those are the top five. But safety and quality are your non-negotiables. Draw a line under them. It's kind of guided a lot of the stuff that we've done. In fact, our huddles, in many cases people still use the phrase safety huddle because safety is the first thing. And now remember, all levels huddle, not just direct performers at Baylor Scott & White. So in the leadership huddles, it used to be, “Any safety concerns?” Crickets, silence. And just like Dr. Toussaint started at ThedaCare, people are going to test this one day and one person says, “Okay, hey, we got this group is 100% clean in all their audits.” And someone raises their hand and says, “We're 100% clean on these audits because we're not doing them right.” So what are you going to do? The leaders, they know it's coming. It's part of the training. “Thank you, thank you for your honesty. Every issue is a process issue. What do we need to do to get done?” And now we've backed it up. So we've gone through the same phases that a lot of other organizations like Toyota and now healthcare organizations have too. First you don't talk about it, then you kind of cover up the problem and then you start talking about the things after they happen. And now we've moved it forward to, in a lot of organizations do this, the concept of great catches, catching those little safety and quality things and rewarding those individuals well before. So an example, way before a fall, there was a trip hazard, right? It's a great catch. Way before there's a med error, there's a labeling issue. It's a great catch. So we've now like great organizations are backing this thing up and we've learned a great deal from Baylor. This is where the magic of Scott & White low cost, you know, bending the cost curve, population health is now marrying itself with the great Baylor health system to create Baylor Scott & White Health. And we just learned a great deal both ways. But our culture, we're trying to come up maybe first and foremost with the culture of continuous safety improvement.
Mark Graban: Yeah. And I'm curious also Steve, for your perspectives and then maybe Bob, from a physician standpoint, I know you've brought in other people who had a direct background experience at Toyota. I'm curious what your thoughts, Steve, on their contribution. Coming in as an outsider like it's just a quick aside. I saw somebody sent me a job post for a different Texas health system for director of performance improvement and it said in the job requirements “requires 10 years of healthcare experience.” So, I've got a bias as an engineer and somebody who came from manufacturing just 10 years ago that that hospital is going to filter out a lot of I think the most capable leaders and people who could come in and help them actually improve performance. You guys have done differently. So talk to the benefit of bringing in Toyota folks.
Steve Hoeft: Yeah, we're probably 50/50 as a continuous. Our continuous improvement staff, by the way, is really small. It's a question that a lot of people say. We have about 12 in Central Texas for 16,000 people here. And we're getting more than a thousand ideas implemented every week. So imagine dozens of projects at that level. Same thing in the north. About 12 people. We do have five true sensei. People that are just deep system, they travel a lot. This group, the sensei really have deep Toyota experience. Of the coaches, it's about 50/50, 50% kind of industrial engineers, people that had that manufacturing background and they're usually married or close to somebody with deep clinical background, some nurses and some respiratory technicians, we've really done well both ways. But I do think it's that pure Toyota knowledge that the sensei in this group have that really has been the difference maker. I can't imagine if the philosophy is off 5 degrees and I have a black belt, but if somebody has only that black belt knowledge that it's all about the belt, it's all about statistics, they have to come up with the ideas. That doesn't play well here. There is an emptying of oneself that's required to be a good leader at Baylor Scott & White. You either believe in these people and hired them for more than their hands, or we might as well just quit now. And we learned this from Toyota. And I think at the core that respect for people has to be there.
Mark Graban: Yeah. And I would certainly agree that what I've seen work really well is a combination of outsiders and insiders, nurses and engineers learning from each other, working together. I'm not saying people from manufacturing are the only ones who can help, but I think hospitals hurt themselves by excluding that outside perspective. So Bob as a physician and an executive. What are your thoughts on us outsiders coming in? What are some of your thoughts or experiences around that?
Bob Pryor: Probably one of the more important things that we can do, because if we only hire people that understand the old way of doing things, then how are we ever going to do things differently? So bringing in a different perspective is important. One of the other, I talked about the ABCs of surgery. The other fundamental of medical education is see one, do one, teach one. Well, if you never see one and you never do one, then how can you teach other people how to do it? So going to see how a manufacturing organization applies these techniques is an eye opener for physicians and clinicians, because they go, “Wait a minute, they're actually stopping the line. And that's not the captain that's stopping the line. That's the person who has noticed something is wrong. Now the experts come in and we solve the problem. And then the line starts again.” And you can apply that to what we're doing in the wards. Now we have the rapid response team, where anyone, including a patient's family member, can stop the line and call in the team that looks at it, fixes it, and then the line starts again. But when you see that, it becomes a lot more learnable and teachable than if you just either read it in a book or you come and learn it in a classroom, but having the outside people come in and say, “Let me show you how this works.” Now you've got a framework that says, “I got it. Now let's expand upon that.”
Mark Graban: Yeah. And as we start to wrap up here in a couple minutes, one other thing I wanted to ask you, Bob, we've kind of alluded to the idea of Legacy Scott & White, and then Baylor Scott & White with the merger that occurred about two years ago, Bob, what would you say are some of the strengths and the opportunities that you see as you combine organizations and cultures, or are there any differences in the lean approach that you're trying to reconcile?
Bob Pryor: Well, not necessarily in the lean approach, but in the approach in general. Let me start with that. We had a lot in common. As a matter of fact, before the merger, we had an outside group come in and say they gave us a cultural survey and they said, “These are the two most aligned cultures they'd ever seen prior to merger.” But of course, there were differences. We are drawing from the strength of the Baylor legacy Baylor group that was involved in STEEPCare. Safe, timely, effective, efficient, equitable, and patient-centered. Of course, who can argue with those as goals? They had training classes, and they were fundamentally immersed in STEEPCare. Now, STEEPCare is great, but when you bring Lean and you marry that with STEEPCare, now you get the way to get STEEPCare and you get the way to involve people and you get the way to spread it more than just classes. So the marriage of STEEPCare and Lean has been very good for both organizations.
Mark Graban: Yeah. And for people who might not know that term, there's a book, it's also a Shingo award winner, called Achieving STEEPCare by David Ballard. I've seen Dr. Ballard present at the Society for Health Systems conference. I would recommend people check out that book in addition to newly released the book here by Steve and Bob from CRC Press, The Power of Ideas to Transform Healthcare. So it's a powerful notion. It's a great book with a lot of really practical stories. Steve, maybe to kind of help wrap things up here. Is there a particular story that you can think of that illustrates the power of employee ideas? I know we've been talking about that here in the podcast. But for people who maybe aren't yet convinced that this is such a powerful approach, is there a story or example you like to tell?
Steve Hoeft: Yep, sure. And making heroes out of the everyday people is really the powerful part of this, but I'll use a good example. Mike Sanborn, a great leader, president of Baylor Medical Center, Baylor Scott & White Medical Center, Carrollton. He really wanted to try these idea huddles, but in many cases they're hearing their staff saying, “We already huddle.” So Mike actually gave this story. They got their financial numbers back from the chiefs, and Bob knows who they all are too. And they made money in January. Hooray. They got their volume numbers and their numbers back from March, and somehow he lost money in March, but the volumes were all higher. “How can you lose money in March and made money in January when your volumes are higher?” So and everybody kind of snickered in the leadership group that was coming to see his area that is now a best-practice area. He said, “I want to tell you guys, we're not dumb. We know what we're doing.” Because all the other leaders from another site were snickering. And he said, “We did the math. We sliced this thing up and we realized that it was Medicare outliers, right? We didn't get paid the full amount that we should have been paid for the services rendered. And it was the Medicare portion of this thing. And on top of this, the outliers were basically length of stay.” Now, everybody cringed in the room, right? We still struggle with some length of stay issues and getting people out safely and on time. And Mike said, “So I have two choices right now. I have length of stay issues, Medicare, patients, and some outliers. What would you all do?” And every leader in that room said, “We'd create a committee.” Here's what I said. “I looked at my staff and said, ‘We just started huddling last week. It is way too new. We've only got 12 pilot areas huddling.'” He said, “But let's try it.” He actually said out loud, “I didn't think it would work.” “Let's get the group. We'll get tracking charts in every single area. Let's just let these huddlers on these basic floors start to break this down for on their area. What were the reasons why they didn't get them out on time and how do you solve it?” He said, “We communicated it in less than two days. By the end of the second week, we did not have a single outlier. Not even one.” He said it shocked me. And so he's talked to now Cindy Shamp, one of the other leaders in the north, president of Baylor Scott & White Medical Center, Irving. And she said the same thing to the board of directors in front of the top-notch business leaders of this very large health system and growing. And she said, “I'm going to tell you the reasons why I'm going to spread this. It's not just communication and alignment and engagement. She said, ‘Steve promised and Bob promised that we'd get that and we did.' She said, ‘but we're operating at a new level. We used to get crushed when we hit 87% full. Now we're operating near 100% full and there's no overtime and we're getting leadership development,' she said. ‘And every single department is moving the stick on here now too. We're getting leaders who are skeptical that they could go to the next level and they're getting there quicker because now they're not waiting on just projects. Now they're tapping every idea from every person every day.' When you turn that on, it's just dynamite.”
Mark Graban: And boy, that's dynamite. It's powerful. And I hope your book will open more people's eyes and inspire more people to moving in this direction. So as we wrap up, Bob, do you have a final thought for executives or physician leaders who are maybe still skeptical about this other than reading the book, do you have a key point for them?
Bob Pryor: Sure. It's a journey that's well worth the travel. The journey is one of everybody in the organization picking up their belongings and moving the bar in the direction that healthcare needs to go. Steve used a couple of examples that are really good because there was a lead financial indicator that led to the quality indicator going up. People do not need to languish in a hospital. They need to get well and get out of the hospital, and that is quality. And the balance of all of the things that we do every day sometimes is not apparent. But when you start looking at it in a systematic way, within huddles, within Hoshin Kanri, within making sure the organization is doing what we need to be doing for the benefit of our communities, then people start piling on board. And you're not going to pry this away from them. They're going to continue to make it work.
Mark Graban: Well, Bob, thank you so much for sharing your perspectives here today. And Steve, thank you as well. Again, our guests have been Steve Hoeft and Bob Pryor from Baylor Scott & White Health. The book is titled The Power of Ideas to Transform Healthcare.7 I hope you'll check it out. And thanks again for being here with us today.
Bob Pryor: Thank you.
Steve Hoeft: Thank you, Mark.
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s build a culture of continuous improvement and psychological safety—together. If you're a leader aiming for lasting change (not just more projects), I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s talk.
Join me for a Lean Healthcare Accelerator Trip to Japan! Learn More










Thanks, Dan!
Here is the context of the quote from Dr. Pryor:
[…] Lean has a place in hospitals this is a good posdcast to start with. […]
Comments are closed.